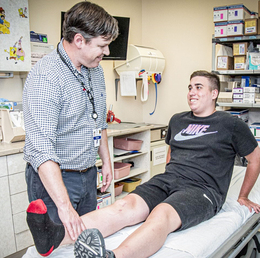
While young children incurring serious knee injuries is not the norm, Shriners Children’s Philadelphia pediatric orthopaedic surgeon Sean R. Waldron, MD, has seen an increase in these incidents over the past decade, particularly among youth athletes.
“I think that’s multifactorial,” Waldron says. “Kids are getting involved in sports at a young age—more kids are playing, so more kids are getting injured. And early sports specialization, we think, can be detrimental in leading to more injuries.”
A knee injury serious enough to lead to surgery or reconstruction is not only difficult for families and young patients to navigate, but also an incredibly scary prospect. That’s why having a surgeon skilled in dealing with pediatric knee injuries—and their additional challenges—is important.
Patient assessment
Once a child is referred to Waldron, things start with X-rays—either ones patients bring with them, or a new order from Waldron.
“They can give you a lot of information about the injury but also since we’re talking about kids, if the child has growth plates that are open, depending on their age, that plays a role in their eventual treatment,” Waldron says.
An injury history is discussed, along with sports and activities in which the child takes part. Lastly are special tests like the Lachman and McMurray tests, maneuvers that manipulate the knee to assess for injury in the anterior cruciate ligament (ACL) and meniscus.
“The ACL is the main stabilizer of your knee joint specifically for twisting and cutting—things that you often do when you’re playing sports. The meniscus is the cushion on the inside of your knee. It’s the shock absorber that protects the cartilage,” Waldron explains.
If an ACL tear is suspected, Waldron will order a MRI to gain accurate pictures of tendons, ligaments and the meniscus. From there, a path of treatment is decided.
Surgery or reconstruction
Twenty years ago, surgeons sought non-operative treatments for youth ACL injuries due to worries of a growth disturbance with a traditional surgery.
“It’s a reasonable concern,” Waldron says, “but the concern for a growth disturbance is outweighed by the risk of damage to the knee by having a torn ACL.”
When Waldron repairs a child’s ACL, he does so by avoiding growth plates and, therefore, circumventing a negative impact to growth. ACL reconstruction is usually what Waldron pursues.
“You have a torn ACL and we’re removing the torn pieces and then making a new ligament from something else, usually a tendon,” he says.
In children younger than 10 years old, that often means using a portion of the iliotibial band—the tendon that runs along the lateral thigh from the pelvis to the side of the knee—to wrap around the inside of the knee and back to front, avoiding drilling any tunnels that could potentially risk growth arrest.
“Then there’s the kid who’s over 10 but still has significant growth remaining. You could still do that one with the iliotibial band, but another option is to drill tunnels in the bone where you avoid the growth plate,” Waldron says. In this reconstruction, the ACL is put at a slightly different angle than normal, using a quadriceps or hamstring tendon to remake the ACL.
Novel to the field is the Bridge Enhanced ACL Repair (BEAR) implant, which is used to aid clotting and healing when the torn ACL is sutured and expected to heal on its own. Waldron is the first to perform BEAR surgery in the city of Philadelphia, having now performed four such surgeries with positive early results.
“Historically we’ve not attempted ACL repair because the fluid inside your knee joint, called the synovial fluid, has the tendency to break down the blood clot that is necessary to heal an ACL repair,” Waldron says.
The BEAR implant can keep that from happening. A collagen scaffold that looks similar to a packing peanut, the implant is placed in the knee joint after surgery, where it protects the repair for about eight weeks and then dissolves.
The device is FDA-approved for children 14 and older with closed growth plates who have injured their ACL within 50 days of surgery. It can, however, be used off-label in younger children.
“We just have to explain to the patients why we think it’s the right thing to do,” Waldron says, adding he’s performed this surgery on a 10-year-old. “Those of us who treat kids know that the younger kids are, the better chance they have of healing things.”
Return to sports
“Return to sports is definitely a hot topic in our field,” Waldron, who also serves as the medical director of Shriners’ motion analysis center, says.
The lab is a “great tool,” historically used for children with cerebral palsy, but also used for sports analysis. Kids who have had ACL surgery undergo a series of tests in the lab to recreate moves they perform in their respective sports. Assessed videos can reveal potential weaknesses and give a baseline for physical therapy.
Because, at the end of the day, Waldron wants to see these kids get back to the sports they love.
“My goal as a surgeon is to get kids back in the game.”
Shriners Children’s Philadelphia
Philadelphia
(215) 430-4000
ShrinersChildrens.org/Philadelphia
Published (and copyrighted) in Suburban Family Magazine, Volume 14, Issue 9.
For more info on Suburban Family Magazine, click here.
For information about advertising in Suburban Family Magazine, click here.
To find out where to pick up your copy of Suburban Family Magazine, click here.